The diagnosis of histamine intolerance is not easy, simply because too much histamine causes symptoms – even in healthy people! The question is always whether the observed reaction is normal, given the ingested histamine dose.
The following tests are used to diagnose histamine intolerance, although some are currently still scientifically controversial and medical guidelines do not recommend using them for now:
- Histamine provocation testing with a histamine solution.
- DAO measurement in the blood (controversial)
- Histamine 50 prick test (rarely used)
- Omission test: histamine elimination diet (recommended1)
- Genetic testing for variants with lower histamine degradation capacity (DAO & HNMT polymorphisms)
Histamine Provocation Testing
In some specialized outpatient clinics, a histamine provocation test is performed by giving the test subjects a solution with a defined amount of histamine to drink, depending on their weight. However, there is a significant risk of life-threatening reactions (swelling of the respiratory tract, drop in blood pressure) that cannot be dismissed. Also, the significance of this test is limited because everyone reacts to histamine – the only question is how strongly. Previous consumption of alcohol, histamine-rich food, or other biogenic amines can also falsify the test result.
The German guideline for histamine intolerance regards histamine provocation testing as possibly helpful in establishing the diagnosis, if the change in diet has been successful.1
Diamine Oxidase Levels in the Blood
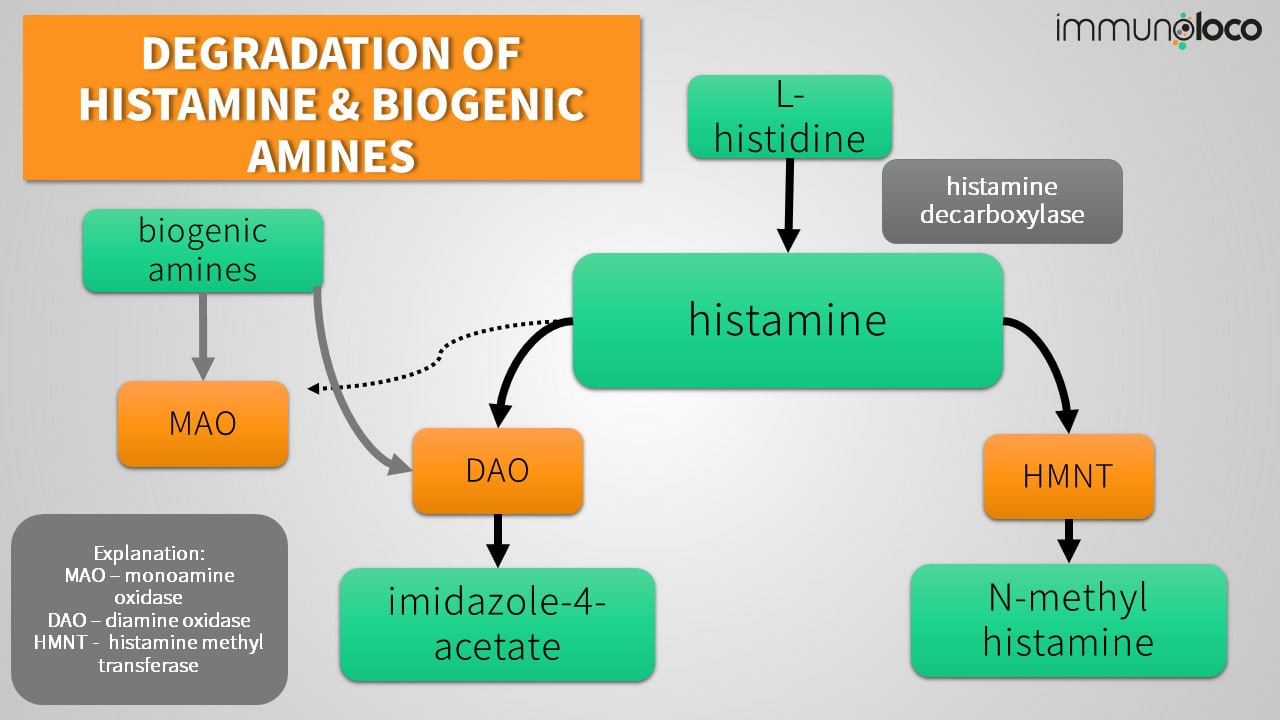
Diamine oxidase (DAO) mainly breaks down histamine ingested from food and is typically found in the intestinal mucosa in the gastrointestinal tract (see causes of histamine intolerance).
Therefore, the diamine oxidase level or DAO serum activity in the blood is sometimes used to diagnose histamine intolerance.
However, the current guideline on histamine intolerance does not consider this measurement sufficiently evidence-based and therefore does not recommend it.1
As things stand, it is also not yet clear to what extent the DAO level or activity of diamine oxidase in the blood is related to the activity and presence of diamine oxidase in the intestine, where the enzyme is most needed to break down biogenic amines.
In some studies, the DAO level in the control group of subjects was also below the defined threshold, although these people did not experience histamine intolerance symptoms. Also, the significance of DAO measurements in the blood as a marker for identifying people who have symptoms after histamine consumption varies from study to study, leading to further doubts about these tests’ usefulness.1
This article is about a health issue. It is important that you have your symptoms examined and treated by medical professionals. This article is not intended to be, and cannot be, a substitute for the care and advice of medical professionals that may be available to you.
Histamine-50-Prick Test
In so-called prick tests performed by an allergist, a control prick test with histamine is usually done. The control patch serves as a comparison for a reaction to one of the other tested substances. It is assumed that histamine usually causes a corresponding skin reaction, e.g., a wheal. The reaction (wheal, redness) on the skin then serves as a control.
In the Histamine 50 prick test, the histamine wheal from an allergy prick test is reassessed after 50 minutes. The underlying assumption is that the wheal’s size should decrease over time due to the breakdown of histamine. An unchanged size would therefore be indicative of a histamine degradation disorder.1
Histamine Elimination Diet: The Best Test & at the Same Time a Therapy.
In the histamine elimination diet, histamine-rich foods are consistently avoided for 14 days. If this leads to a clear improvement of the symptoms, then one can assume a histamine intolerance. In a second step, one should expand the diet step by step to find the personal limit.1,2
In the case of a strict elimination diet, it may also be helpful to omit other foods containing biogenic amines. These require the same enzymes for degradation in the body as histamine, like diamine oxidase (DAO).2
Genetic Testing in Cases of Suspected Histamine Degradation Disorder
In the case of severe symptoms, genetic tests can be carried out to see whether variations in the genes that are jointly responsible for histamine breakdown in the body are present. These variations, called polymorphisms, occur naturally, and many are not classified as pathological and disease-causing.
But certain genetic variations in the DAO gene, for example, in the sequence variants rs2052129, rs2268999, rs1049742, and rs10156191, are associated with reduced DAO activity. Thus, the body is less able to break down the histamine produced.3–5
In addition to diamine oxidase, histamine methyltransferase, or HMNT, is responsible for degrading histamine. Polymorphisms can also be present here. The HNMT C314T genotype results in a 30-50% reduction in histamine methyltransferase activity and is more common in people with aspirin intolerance (AERD), for example.6,7
Depending on the cause of the histamine intolerance syndrome (HIS), the treatment approaches differ. In the case of genetic polymorphisms, it is often sensible to ensure that the histamine-degrading enzymes DAO and HNMT are not additionally blocked in their activity by certain drugs, if not medically necessary.
Fecal Histamine Testing: Non-Specific and rather a Dysbiosis Marker
Histamine in stool is generally not a specific marker for histamine intolerance. There may be histamine or other biogenic amine-forming bacteria in the intestine that produce high histamine levels in stool depending on their composition or if the bacteria have overgrown.8
Therefore, a high histamine level in the stool is more indicative of a possibly unfavorable composition of the intestinal flora and does not necessarily have to be associated with histamine intolerance.
However, an overgrowth of histamine-forming bacteria can increase the amount of histamine produced in the body and overload the degradation capacity. These unfavorable processes, in turn, can lead to histamine-mediated symptoms.8
Urinary Methylhistamine: Elevated in Gastrointestinal Allergies and Mast Cell Disease.
Urinary methylhistamine is also not a specific marker for histamine intolerance and does not help diagnose histamine intolerance. Instead, elevated methylhistamine may indicate an allergy in the gastrointestinal tract or mast cell diseases, such as mast cell activation syndrome (MCAS) or mastocytosis.9
Interested in more information & knowledge?
Every now and then, and only when there’s something interesting for you. Currently less than once a month, but packed with information – unsubscribe at any time and free of charge.
Who is affected by histamine intolerance?
Around 80% of patients affected by histamine intolerance are female, and between 25 and 45 years old. Affected women often report a cycle-dependency of their symptoms, so a link to sex hormones is assumed.1,2
In severe cycle-dependent symptoms, gynecologists sometimes prescribe “the pill” in the long-term cycle with fewer breaks to regulate or stop the monthly bleeds. However, it is not uncommon that oral contraceptives (“the pill”) are not well tolerated in sensitive women with intolerances.
During pregnancy, an improvement in histamine intolerance-related symptoms can often be observed, as diamine oxidase, responsible for the breakdown of histamine, increases many times over. This increase protects the unborn child from histamine excess.10
You want a little more support? Maybe there is something for you here! And if you want to support me, then I am very happy if you consider to buy me a coffee. Thanks in advance!
References
- Reese I, Ballmer-Weber B, Beyer K, et al. German guideline for the management of adverse reactions to ingested histamine: Guideline of the German Society for Allergology and Clinical Immunology (DGAKI), the German Society for Pediatric Allergology and Environmental Medicine (GPA), the German Association of Allergologists (AeDA), and the Swiss Society for Allergology and Immunology (SGAI). Allergo J Int. 2017;26(2):72-79. doi:10.1007/s40629-017-0011-5
- Maintz L, Novak N. Histamine and histamine intolerance. Am J Clin Nutr. 2007;85(5):1185-1196. doi:10.1093/ajcn/85.5.1185
- García‐Martín E, Martínez C, Serrador M, et al. Diamine Oxidase rs10156191 and rs2052129 Variants Are Associated With the Risk for Migraine. Headache: The Journal of Head and Face Pain. 2015;55(2):276-286. doi:https://doi.org/10.1111/head.12493
- Agúndez JAG, Luengo A, Herráez O, et al. Nonsynonymous polymorphisms of histamine-metabolising enzymes in patients with Parkinson’s disease. Neuromolecular Med. 2008;10(1):10-16. doi:10.1007/s12017-007-8017-7
- Meza-Velázquez R, López-Márquez F, Espinosa-Padilla S, Rivera-Guillen M, Ávila-Hernández J, Rosales-González M. Association of diamine oxidase and histamine N-methyltransferase polymorphisms with presence of migraine in a group of Mexican mothers of children with allergies. Neurologia. 2017;32(8):500-507. doi:10.1016/j.nrl.2016.02.025
- Kim S-H, Kang Y-M, Cho B-Y, Ye Y-M, Hur G, Park H-S. Histamine N-methyltransferase 939A>G polymorphism affects mRNA stability in patients with acetylsalicylic acid-intolerant chronic urticaria. Allergy. 2009;64:213-221. doi:10.1111/j.1398-9995.2008.01795.x
- Parejo PA, García-Agúndez JA, Cornejo-Garcia JA, et al. Association Study of Functional Polymorphisms in Genes Involved in Histamine Homeostasis and Multiple NSAID–Triggered Urticaria and/or Angioedema and Anaphylaxis in Patients without Pre-Existing Chronic Urticaria (MNSAID-UA). Journal of Allergy and Clinical Immunology. 2013;131(2):AB169. doi:10.1016/j.jaci.2012.12.1266
- Schink M, Konturek PC, Tietz E, et al. Microbial patterns in patients with histamine intolerance. J Physiol Pharmacol. 2018;69(4). doi:10.26402/jpp.2018.4.09
- Raithel M, Hagel A, Albrecht H, et al. Excretion of urinary histamine and N-tele methylhistamine in patients with gastrointestinal food allergy compared to non-allergic controls during an unrestricted diet and a hypoallergenic diet. BMC Gastroenterology. 2015;15(1):41. doi:10.1186/s12876-015-0268-4
- Maintz L, Benfadal S, Allam J-P, Hagemann T, Fimmers R, Novak N. Evidence for a reduced histamine degradation capacity in a subgroup of patients with atopic eczema. J Allergy Clin Immunol. 2006;117(5):1106-1112. doi:10.1016/j.jaci.2005.11.041
[simple-author-box]
Immunoloco unterstützen
immunoloco möchte Betroffenen kostenlos gute und hilfreiche Informationen rund um ein verrücktes Immunsystem bieten. Du findest das gut? Dann unterstütze immunoloco und meine Arbeit doch gerne. Jeder Euro zählt und hilft, das Projekt weiterleben zu lassen.

Dear Lisa
Please could you do an article on intolerance to Salicylates, Thiols, Phenols and Amines
Thank you 🙂
Dear Amanda,
I am already on it – especially phenols and salicylates. 🙂
Thank you for the encouragement – it is a complicated topic and therefore I really appreciate the comment!